As previously mentioned, the percentage of air present in consolidated lung is only around 10%. This means lung US, like in pneumothorax, does not rely on air/fluid artefacts but can image the pathology directly. Alveolar syndrome encompasses alveolar consolidation (fluid in the alveoli - infection, blood) and atelectasis (collapsed alveolar units secondary to bronchial obstruction (dynamic airway compression from weakened distal airways or reduced FRC or compression by surrounding effusion). Severe alveolar oedema does not cause a fully consolidated US appearance - there may be small areas of consolidation but the lung will not appear hepatisised.
Consolidation
The multiple fluid filled alveolar units are separated by interlobular septa. If a consolidation reaches the chest wall (which over 90% do), the US beam will penetrate into the lung and be reflected back by each interlobular septa creating a tissue like pattern which looks much like the liver does on US.
Placing the probe at the PLAPS point discovers 90% of consolidations (90% sensitive and 98% specific) but more liberal use of the prove over the chest will improve the sensitivity further.
Lung sliding is often not present due to reduced lung expansion and sticking of the pleura due to an inflammatory process.
2 patterns are seen with consolidation:
Tissue-like sign.
As above the consolidated lung will be ‘hepatisised’ (looks similar to liver).
Extensive consolidation (of a whole lobe) will allow the opposite plural line to be seen (8-11cm deep) with mediastinum deeper still with the aorta or IVC visible. A fully consolidated lobe may be seen floating in a pleural effusion.

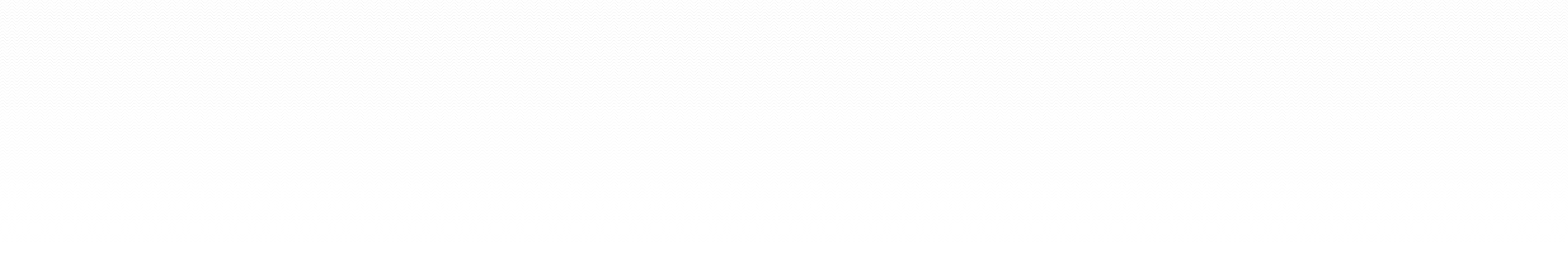
A fully consolidated right lower lobe surrounded by an effusion. IVC visible.
Shred sign.
Here it looks as if a chunk or chunks have been taken out of the lung (echo poor areas). These chunks will be bordered by aerated lung identified by sliding and comets.
This is most suggestive of pneumonia. The border of the consolidated and aerated lung is not sharp.
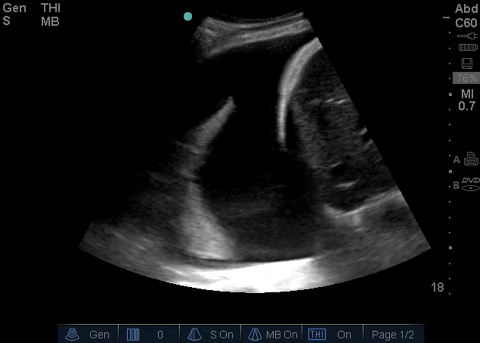
The shred sign. There appear to be chunks missing from the lung base.
Assessing degree of consolidation / aeration
If a lobe is not completely consolidated then the transition from aerated to consolidated lung is often seen with respiration when the probe is in a fixed position. This is not because the consolidated bit of lung is filling with air but because an aerated area is moving into view.
Anterior consolidations
Often small.
Often have adjacent B lines.
If infective are more likely to have an indistinct boundary with peri-lesional B lines and deep comets (not technically B lines as do not arise from the pleura) deep to the far margins. A focal interstitial syndrome.
If infarcts (PE) then are characteristically wedge shaped with sharp margins.
Anterior consolidation in a patient with legionella pneumonia.
More severe anterior consolidation in the same legionella patient with the probe in a different location (all lobes of both lungs were affected to varying degrees).
Air bronchograms
These are white. They may be present in a consolidation or not so are specific but not sensitive and are present within an already highly specific sign. They are punctiform if transverse to the beam and linear if longitudinal. An air bronchogram which moves with respiration means that there is no bronchial obstruction and helps distinguish between consolidation and atelectasis (but not very well). Don’t mistake a bronchogram which appears and disappears (being moved by surrounding lung) with one which moves (gas flow within it moves it towards the periphery) This can be demonstrated with M-mode (and looks similar to the sinusoid sign). Static bronchograms make atelectasis more likely. Dynamic air bronchograms make pneumonia more likely.
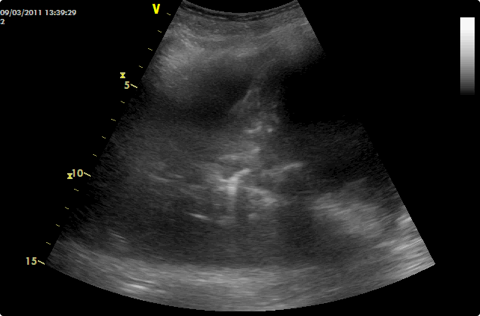
Dynamic air bronchograms
Fluid bronchograms
These are black (as they contain fluid). They are probably specific to pneumonia (expert opinion).
They can be distinguished from vessels by colour doppler and the angulation of their branches.
Combination of air and fluid bronchograms in a consolidated lower lobe.
Punctiform air bronchograms (the bright white blebs) and fluid bronchograms (black) in a consolidated lower lobe. There is aerated lung present at the depths of the image.
Vascular pattern
In neoplasia there will be increased vascularity with a disorganised appearance.
Vascularity is normal in consolidation.
Abscesses and necrosis
Scanning through the full volume of a consolidation will reveal if an abscess or necrosis is present. Straight forward consolidation has the tissue like pattern described above (with or without air bronchograms) whereas a necrotic area or abscess will appear as a hypoechoic, fairly regular, area. An air fluid level may be seen.
Areas of necrosis are detected better than with CT.
Atelectasis
This looks very similar to consolidation with a tissue-like appearance. Non dynamic air bronchograms are suggestive (see above) but these are also present in 40% of cases of pneumonic consolidation.
In obstructive atelectasis non dynamic air bronchograms will initially be present and then disappear as the air gets resorbed.
Fluid bronchograms are a feature of pneumonia and not atelectasis.
Almost all pleural effusions in critically ill patients will show consolidated/atelectatic lung underneath. Distinguishing the 2 can be done by tapping the fluid and seeing if the consolidation/atelectsis is improved (which it won’t be with consolidation).
If the atelectasis is large (such as lobar collapse) there will be the expected associated signs of loss of volume such as raised hemidiaphragm and mediastinal shift (heart visible at right parasternum).
Other signs of atelectasis:
Absence of lung sliding
The lung pulse (also called T-lines). Cardiac motion vibrates the motionless lung in time with contractions. This also rules out pneumothorax.
T-lines in an ARDS patient without lung sliding (no consolidation here).
Diaphragm
The diaphragm is easily visualised if there is basal consolidation or an effusion. It is not clearly seen with normally aerated lung but will be identified by air above (on the left of the screen) and abdominal organs below (on the right).
The diaphragm is raised if above the normal phrenic line defined by the BLUE hands.
The normal inspiratory amplitude longitudinally is between 15-20mm.
Low amplitude reflects atelectasis, low tidal volume or raised intra-abdominal pressure. Amplitude is not affected by effusion.
Paradoxical movement indicates phrenic nerve palsy (this will also abolish lung sliding, elevate the diaphragm and show absence of inspiratory thickening).
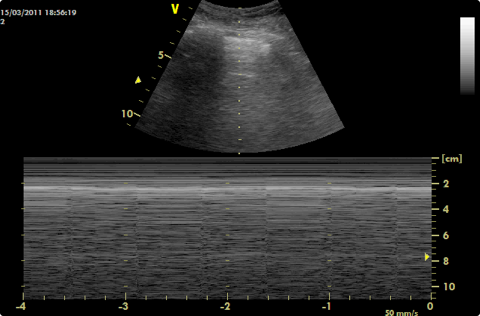
The right diaphragm is clearly visible between liver and effusion and its thickness can even be measured. A moving image will allow excursion to be measured.
Lung punctures
This may provoke anxiety but is advocated by Lichtenstein with sound reasoning.
Accurate microbiological diagnosis is very important.
The organisms will be within the lung tissue.
If the needle is inserted into a consolidated lung the risk of pneumothorax will be very small.
If lung sliding is absent it suggests the pleura are adherent further lowering the risk of pneumothorax.
Each case should be done on a balance of risk/benefit.
Suggested criteria for lung puncture:
Benefit outweighs risk.
Large consolidation at accessible site.
Abolished lung sliding.
Air bronchograms absent of far from needle site.
Use a 21G needle. Need to pull the plunger back hard and will only get a drop of material back. Will need the cooperation of your micro department for this proceedure.
Check with US for a pneumothorax post proceedure.
Lichtenstein says the above criteria mean a pneumothorax never happens and that the tap is positive in around 50%.
Discussion with a chest physician who wrote the BTS guidelines for management of pneumothorax agrees that this is a safe procedure in his opinion.
2012 Consensus Evidence-based Recommendations (Consolidation)
Intensive Care Med (2012) 38:577–591
Signs and clinical implications
B-D3-S1 (strong: level C)
The sonographic sign of lung consolidation is a subpleural echo-poor region or one with tissue-like echotexture.
Lung consolidations may have a variety of causes including infection, pulmonary embolism, lung cancer and metastasis, compression atelectasis, obstructive atelectasis, and lung contusion. Additional sonographic signs that may help to determine the cause of lung consolidation include the following:
- The quality of the deep margins of the consolidation
- The presence of comet-tail reverberation artifacts at the far-field margin
- The presence of air bronchogram(s)
- The presence of fluid bronchogram(s)
- The vascular pattern within the consolidation.
B-D3-S4 (strong: level A) Lung ultrasound for detection of lung consolidation can be used in any clinical setting including point-of-care examination.
B-D3-S8 (strong: level A)
Lung ultrasound should be used in the evaluation of lung consolidation because it can differentiate consolidations due to pulmonary embolism, pneumonia, or atelectasis.
P-D3-S6 (strong: level B)
Lung ultrasound is a clinically useful diagnostic tool in patients with suspected pulmonary embolism.
P-D3-S7 (strong: level A)
Lung ultrasound is an alternative diagnostic tool to CT in diagnosis of pulmonary embolism when CT is contraindicated or unavailable.
P-D3-S3 (strong: level B)
Lung ultrasound is a clinically useful tool to rule in pneumonia; however, lung ultrasound does not rule out consolidations that do not reach the pleura.
B-D4-S8 (strong: level C)
Lower-frequency ultrasound scanning may allow for better evaluation of the extent of a consolidation.
Imaging strategies and learning curve
B-D3-S5 (strong: level A)
Lung ultrasound should be considered as an accurate tool in ruling in lung consolidation when compared with chest radiography.
B-D3-S6 (strong: level B)
Lung ultrasound may be considered as an accurate tool in ruling out lung consolidation in comparison with chest radiography.
B-D3-S7 (no consensus: level C)
Use of lung ultrasound as an initial diagnostic strategy in the evaluation of lung consolidation improves outcomes in comparison with chest radiography.
B-D3-S3 (strong: level N/A)
Ultrasound diagnosis of lung consolidation may be considered as a basic sonographic technique with a steep learning curve.
B-D4-S6 (strong: level B)
Lung ultrasound should be considered in the detection of radio-occult pulmonary conditions in patients with pleuritic pain.
B-D3-S2 (weak: level C)
In the evaluation of lung consolidation, the sonographic technique should commence with the examination of areas of interest (if present, e.g., area of pain) then progress to the entire lung, as needed.
B-D4-S3 (strong: level A)
In mechanically ventilated patients, lung ultrasound should be considered because it is more accurate than chest radiography in distinguishing various types of consolidations.
B-D4-S4 (strong: level A)
In mechanically ventilated patients lung ultrasound should be considered as it is more accurate than portable chest radiography in the detection of consolidation.
B-D4-S9 (no consensus: level N/A)
Lung ultrasound is accurate in distinguishing various types of consolidations in comparison with CT scan in mechanically ventilated patients.